
STIs: Top 5 Practical Things To Know
STIs or Sexually Transmitted Infections are gaining terrain right now, and for me, part of this is the lack of education surrounding sexual health. STIs are something to be afraid of, and they aren’t death sentences; they are easily treated. So, let’s dive into this blog and learn some of the practical things everyone should know about STIs.
1. Protecting yourself

When you have a new partner, it’s essential to protect yourself. Even if the person is confident and you trust them, you can only be truly safe if you get tested together. Before that, a condom is a must to avoid the risk of contracting an STI during sex.
Be careful; fellatio without a condom is also a risky practice since the AIDS virus or the chlamydia bacteria are transmitted through the seminal fluid (common at the beginning of an erection) and through the semen.
For optimal protection, condoms should be used at the beginning of foreplay. Some sexual caresses can also be contaminated. When in doubt, or if a condom is not available, abstinence is the best protection before getting tested…
2. Observe some hygiene rules

Be especially careful when trying on swimwear or underwear in a store:
- Keep your underwear on for protection.
- Never borrow a friend’s razor.
- Be aware that drug use carries risks of contamination. The transmission of certain STIs or STDs can also occur by sharing contaminated linen, even if it is quite rare.
Sharing snorting equipment such as straws carries a risk of infection by bacteria, viruses, and fungi. The highest risk is that of sharing injection equipment such as syringes, where the transmission of the AIDS virus, syphilis, and hepatitis is frequent. This is the case with cocaine use, which is increasingly widespread in the United States, especially among young people.
3. Get tested regularly
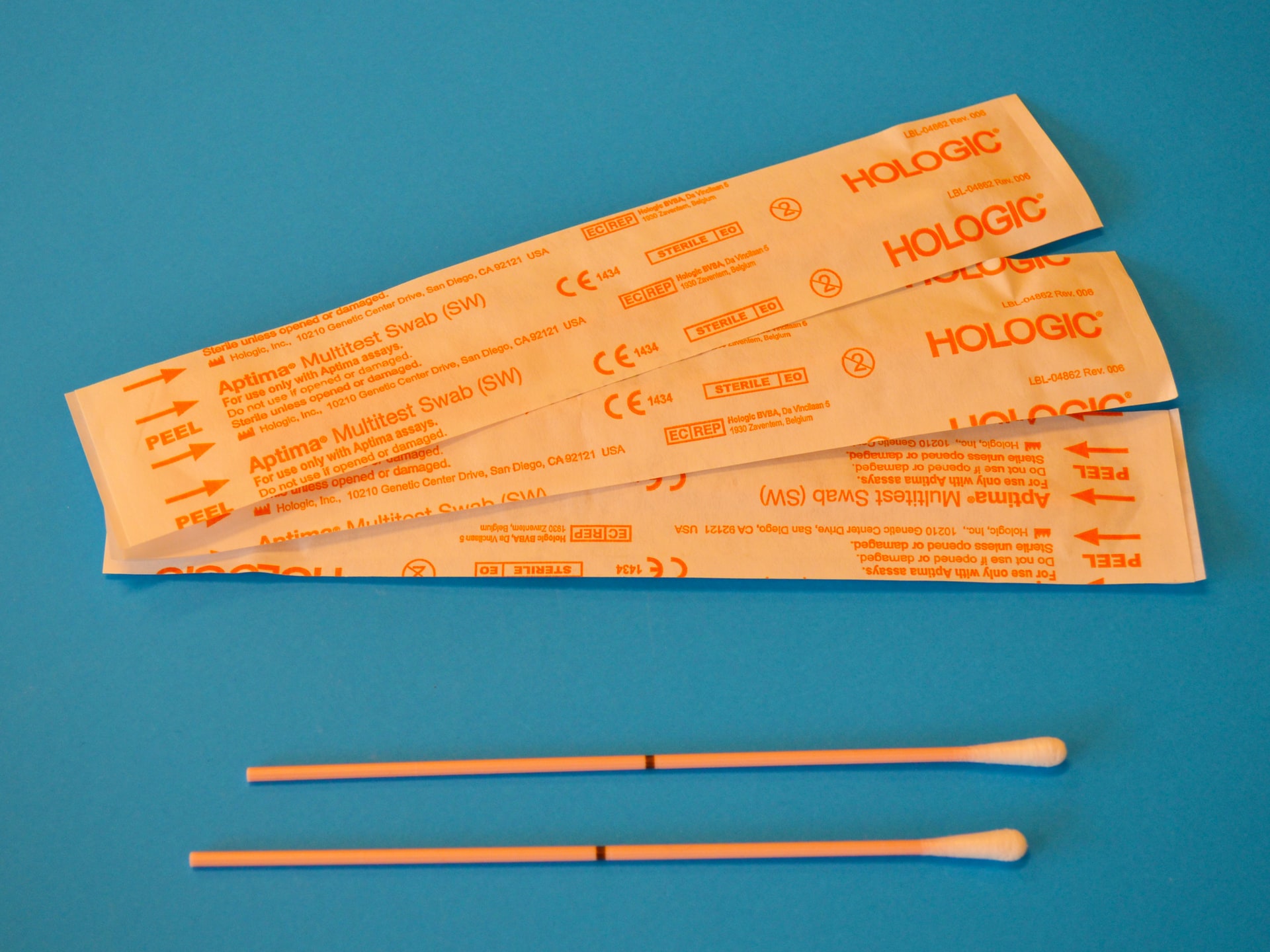
In order to be able to manage a possible STI, it is essential to get tested regularly. Having a Pap smear every two years at the gynecologist’s office can also detect HPV in case of doubt. It is necessary to ask for it. Be aware that fidelity in a couple does not prevent the arrival of this virus, which can have an incubation time of several years and sometimes be associated with an autoimmune disease.
Your gynecologist will still be able to make a diagnosis if you come to see him because of irregular discharge, pain during urination, small pimples, or itching that may be symptoms of an STI. A simple urine test will also detect the presence of chlamydia, and there are several screening tests for the AIDS virus.
You can be tested for free at your local Plan Parenthood (screening and diagnostic center), in associations, on authorized mobile devices, or in a medical analysis laboratory. You can also buy a self-test in a pharmacy if you have been at risk for HIV after having sex for more than 3 months.
4. Getting vaccinated against certain STIs

Unfortunately, there is still no vaccine against the AIDS virus, mononucleosis- also known as kissing disease- oral or genital herpes, or chlamydia. But there is an effective vaccine against hepatitis B, a highly contagious and incurable liver disease.
This vaccine, which is controversial because of its potential side effects, can nevertheless prevent this serious and widespread STI. It is also possible with a vaccine to prevent the majority of papillomaviruses, responsible for cervical cancer and infertility in women. This vaccine is most effective when given in adolescence.
5. Get treatment and tell your partners

Some STIs can be treated. Syphilis, chlamydia, and gonorrhea (known as “hot piss”) can be treated with antibiotics over varying lengths of time. It is necessary to react quickly in the case of chlamydia which can cause sterility in women. Herpes is incurable, but antiviral drugs can relieve the attacks.
Condylomata can be removed in the hospital by electrocoagulation. In any case, it is important to warn your partners so that they can be tested, get treatment if they have contracted the STI, and not transmit it to you or their future partners.
You should also know that there is an emergency treatment available if you have taken a risk with someone who has HIV, if you did not protect yourself or if the condom failed. This is called PrEP or pre-exposure prophylaxis and should be taken no later than 48 hours after intercourse. Go to your nearest emergency room to get it.
Remember, if you need more information go see your local medical practitioner or to the local Plan Parenthood. Sound off in the comments section below and let us know what you want to read next and if you want to read more about STIs.
You May Also Like

The Majestic Blue Heron: A Symbol of Grace and Serenity
2023-05-26
Debunking the Myth: The Science Behind the 10% Brain Usage Fallacy
2023-09-25

One Comment
Pingback: