Top 5 Things To Know About Monkeypox
To date, the United Kingdom has reported nine cases of Monkeypox, an infectious disease that is not easily transmitted to humans. The first case, identified on May 7, 2022, occurred in a traveler returning from Nigeria. A week later, two other people were diagnosed with Monkeypox, but investigations by health authorities found no link to the initial case. First-generation smallpox vaccines are no longer available to the general public. A newer vaccinia-based vaccine was approved for smallpox and monkeypox prevention in 2019, but it is not yet widely available.
Six more cases have been diagnosed in the United Kingdom, with no clear link between them, raising concerns about the circulation of the virus in the population, although the risk of human-to-human spread is likely to be low, except in cases of close physical contact. Since then, several dozen cases have been confirmed in the United Kingdom and various European Union countries, and more cases are under investigation.
Until now, cases of Monkeypox have been rare outside of West and Central Africa; two cases were identified in the United States last year, both in travelers returning from Nigeria. But the case identified recently in Massachusetts occurred in an adult who had traveled to Canada. Here are five things to know about this potentially deadly disease.
1. Monkeypox is caused by a virus similar to smallpox

Monkeypox (also known as simian orthopox) is caused by a virus of the same name that is closely related to smallpox, which has now been eradicated from the world. Both are members of the genus Orthopoxvirus in the family Poxviridae. Monkeypox was first discovered in 1958 when outbreaks of disease-causing smallpox-like symptoms were found in monkeys kept in captivity for research.
It was first observed in humans in 1970 in the Democratic Republic of Congo (DRC) and is now endemic in central and western Africa. As of 2020, the World Health Organization (WHO) has recorded 4,594 suspected cases of Monkeypox, resulting in 171 deaths (case-fatality rate of 3.7%). These cases were listed as suspected because confirmation requires a PCR test, which is not readily available in endemic areas.
2. Monkeypox causes pustules all over the body
Symptoms usually appear between five and 13 days after infection, but the incubation period can last up to 21 days. The disease begins with fever, headache, muscle aches, back pain, swollen lymph nodes, chills, and severe fatigue. The rash appears after the onset of the fever. The rash is initially limited to the face, palms, and feet before spreading to other parts of the body and sometimes even to the oral mucosa, genitals and cornea.
It progresses to vesicles, then pustules, until it forms a crust that eventually falls off, in some cases causing large areas of skin to peel off. Generally, healing is spontaneous, and symptoms subside spontaneously within a month, but in some circumstances, the disease can be fatal in one in ten cases. Children are particularly vulnerable.
3. Diagnosis requires PCR testing
Since many diseases, such as chickenpox and measles, are accompanied by a rash, a definitive diagnosis can only be made by specialized laboratories. Indeed, as recommended by the WHO, PCR testing is required, as the antigens of orthopoxviruses and the antibodies they induce cannot accurately determine whether it is monkeypox virus or other related viruses.
4. Monkeypox is spread by close contact
The virus is usually transmitted to humans from infected wild animals (rodents, primates) living in the tropical forests of central and western Africa, but human-to-human transmission is also possible. As with the Ebola virus, it is only through close contact with lesions, body fluids, respiratory droplets of infected patients, or contaminated materials such as bedding or clothing.
5. There is currently no treatment, but we do have a (very old) vaccine

Currently, WHO does not recommend any specific treatment for Monkeypox, but some antivirals, such as tecovirimat, are approved for use against orthopoxviruses. The smallpox vaccine that led to the eradication of smallpox several decades ago is highly effective against Monkeypox (estimated efficacy of 85%). But this first-generation vaccine is no longer available to the population. A newer vaccine, also prepared from vaccinia, was approved in 2019 for the prevention of smallpox and Monkeypox, but its availability is still limited.
Sound off in the comments section below, and tell us what you want to read next and if you want to read more about Monkeypox.
You May Also Like

Top 5 Tips To Fight Seasonal Depression (Part 2)
2023-01-18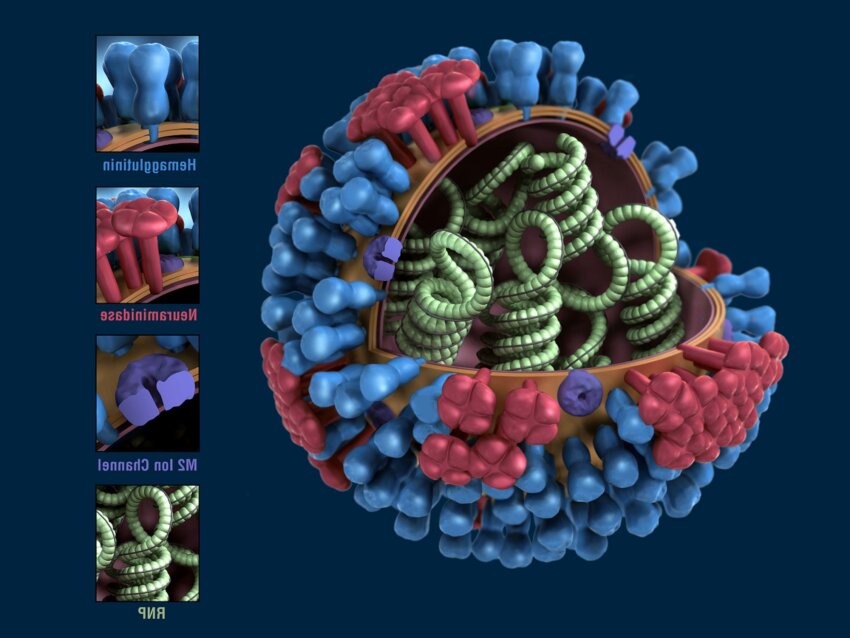
What Are the 3 Types of Influenza
2022-03-05